The history of healthcare communication truly shows how quickly the industry evolves to cater to the needs of patients and providers alike. It has come a long way since its earliest forms. Before the digital age, communication between healthcare providers was rudimentary. In the early 90s, a physician’s main tools for inter-provider communication were the landline telephone and postal mail. While these methods allowed for the exchange of patient information, they were far from efficient. The delay in sending letters and the challenge of coordinating phone calls during office hours made real-time collaboration nearly impossible. Physicians had to balance the need for communication with the immediate demands of patient care, often sacrificing one for the other.
The Evolution to Digital Communication
We know modern healthcare technology is impressive, but it hasn’t always been that way. From paper charts to fully automated AI programs, let’s take a look at just how far the industry has come.
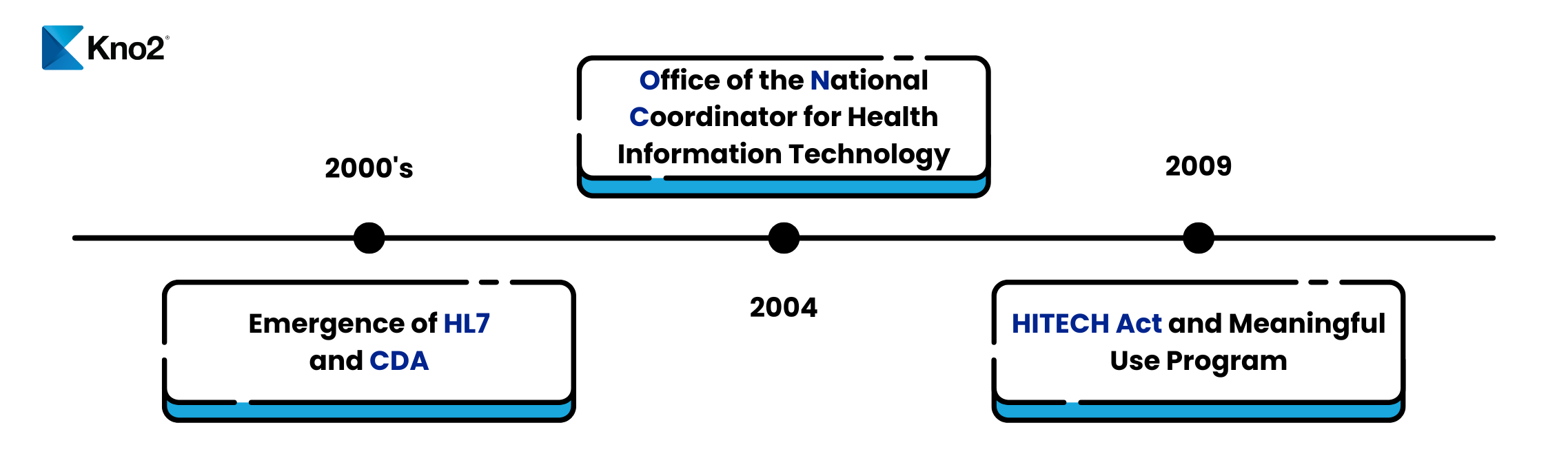
Early Milestones in Healthcare Communication
1960s-1970s: The Birth of EHRs: The concept of electronic health records began to take shape in the 1960s. Early efforts were primarily focused on automating administrative tasks rather than clinical documentation. For instance, the problem-oriented medical record (POMR) system, developed in the late 1960s, was one of the first attempts to structure medical records electronically.
1980s: Initial Steps Towards Standardization: The 1980s saw the development of some of the first standards for health information exchange. The Continuity of Care Record (CCR) standard was designed to facilitate the exchange of patient information between providers. However, adoption was limited, and true interoperability remained elusive.
1996: HIPAA and the Push for Standardization: The Health Insurance Portability and Accountability Act (HIPAA) of 1996 was a significant legislative milestone. While HIPAA is best known for its privacy and security provisions, it also included requirements for the standardization of electronic health transactions. This laid the groundwork for more robust interoperability standards.
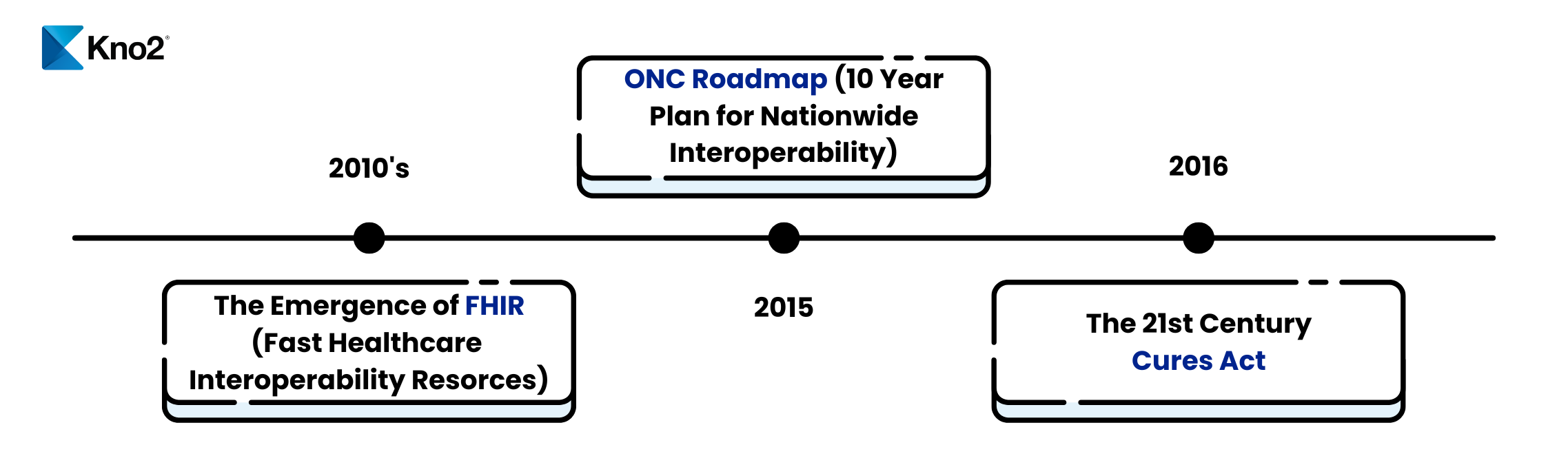
The Rise of Interoperability Standards
2000s: The Advent of HL7 and CDA: Health Level Seven International (HL7) emerged as a critical player in developing interoperability standards. HL7’s Clinical Document Architecture (CDA), introduced in the early 2000s, provided a framework for the exchange of clinical documents. CDA was a significant step forward, enabling more structured and semantically rich data exchange.
2004: The Office of the National Coordinator for Health Information Technology (ONC): The ONC was tasked with promoting the adoption of health information technology and advancing interoperability. This federal involvement spurred numerous initiatives aimed at improving health information exchange.
2009: The HITECH Act and Meaningful Use: The HITECH Act of 2009 provided significant financial incentives for the adoption of EHRs through the Meaningful Use program. Meaningful Use criteria required healthcare providers to demonstrate that they were using EHRs in ways that improved patient care. Interoperability was a key component of these criteria, driving further advancements in data exchange capabilities.
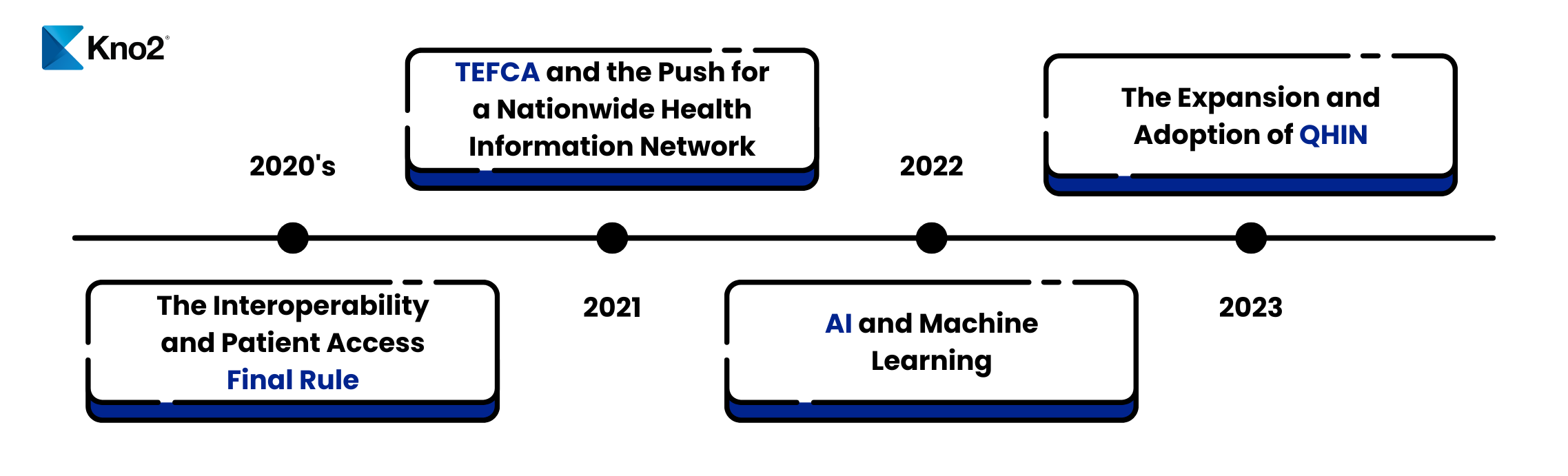
Modern Advances in Interoperability
2010s: The Emergence of FHIR: Fast Healthcare Interoperability Resources (FHIR), developed by HL7, represented a major leap forward in interoperability. Introduced in 2012, FHIR was designed to be a more flexible and modern standard for exchanging healthcare information. It leveraged web-based technologies and was easier to implement than previous standards, facilitating more seamless data exchange.
2015: The Interoperability Roadmap: The ONC released the Shared Nationwide Interoperability Roadmap, outlining a ten-year plan to achieve nationwide interoperability. The roadmap emphasized the importance of standardized APIs, data standards, and the need for a supportive policy and technical infrastructure.
2016: The 21st Century Cures Act: The 21st Century Cures Act included provisions to advance interoperability and prevent information blocking. It mandated the development of standardized APIs to enable patients to access their health information electronically, further pushing the healthcare industry toward more open and accessible data exchange.
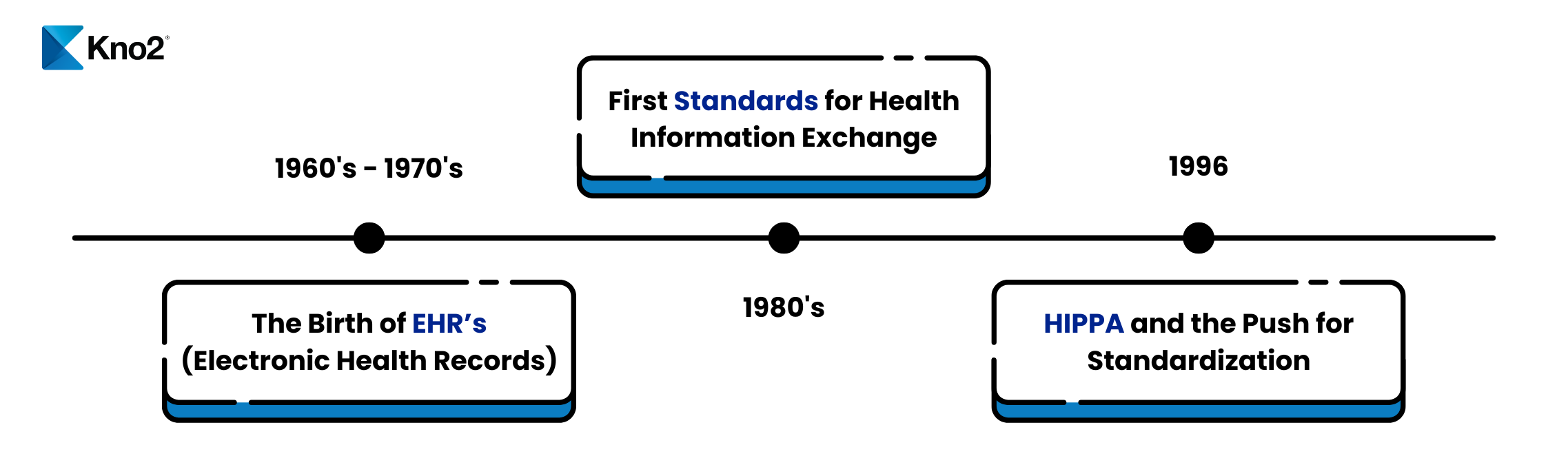
The Current State of Interoperability
2020s: The Interoperability and Patient Access Final Rule: The Centers for Medicare & Medicaid Services (CMS) and the ONC finalized rules aimed at improving interoperability and patient access to health information. The rules required healthcare providers and payers to implement standardized APIs. This allows patients to access their data using third-party applications securely.
2021: TEFCA and the Push for a Nationwide Health Information Network
The Trusted Exchange Framework and Common Agreement (TEFCA) was introduced to establish a single on-ramp to nationwide interoperability. TEFCA aims to create a standardized framework for health information exchange, ensuring that data can flow seamlessly across different networks and systems. This outlined the role and requirements for QHINs (Qualified Health Information Networks)
2022: The Role of Artificial Intelligence and Machine Learning: As we move further into the 2020s, artificial intelligence (AI) and machine learning (ML) are playing an increasingly important role in healthcare interoperability. These technologies have the potential to analyze vast amounts of health data, identify patterns, and facilitate more efficient data exchange. AI-driven interoperability solutions are helping to bridge the gaps between disparate systems and improve the overall quality of patient care.
2023 and Beyond: The expansion and adoption of QHINs continued, with ongoing efforts to integrate them into the broader health information exchange system. This period focuses on increasing the number of certified QHINs and ensuring their effective implementation to support nationwide interoperability. Every QHIN has to agree to share data and collaborate for the good of patient care. To this day, there are only five QHINs, Kno2 being one. QHIN was/is a huge leap forward toward true interoperability.
Challenges and Future Directions
Despite the significant progress made, several challenges remain in achieving true healthcare interoperability. These include:
- Data Privacy and Security: Ensuring that patient data is exchanged securely, and that privacy is maintained is a critical concern. As interoperability increases, so does the potential risk of data breaches and unauthorized access.
- Standardization: While significant strides have been made in developing standards, the adoption and consistent implementation of these standards across all healthcare systems remain a challenge.
- Cultural and Organizational Barriers: Interoperability requires not only technological solutions but also changes in organizational culture and practices. Healthcare providers must be willing to share data and collaborate for the greater good of patient care.
- Economic Considerations: Implementing interoperability solutions can be costly, and the return on investment is not always immediately apparent. Healthcare organizations must weigh the costs and benefits carefully.
Looking Ahead
The future of healthcare interoperability holds great promise. Emerging technologies have the potential to revolutionize data exchange by providing secure, transparent, and immutable records. Additionally, the continued development of AI and ML will further enhance the ability to analyze and exchange health information.
As the healthcare industry continues to evolve, the focus must remain on developing and implementing solutions that prioritize patient care, data security, and seamless information exchange. The journey towards full interoperability is ongoing, but the progress made so far provides a strong foundation for a more connected and efficient healthcare system.
Although it’s not perfect yet, the timeline of healthcare interoperability is a testament to the relentless pursuit of better patient care through improved communication and data exchange. From the early days of landline phones and postal mail to the modern era of interoperability solutions, each milestone has brought us closer to a future where healthcare providers can collaborate in real time, leading to better outcomes for patients everywhere. Through it all, Kno2 will continue to fight for the interoperability of the future.