One of its overarching goals of the 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act, which was part of the American Recovery and Reinvestment Act, was to require providers to move from paper to electronic documentation in order to make it easier to exchange patient information and coordinate care.
We are largely there, at least in terms of hospitals and physician offices. More than 95 percent of hospitals and nearly 90 percent of office-based physicians, have adopted an electronic health record (EHR) system.
While that is great news, the reality is that patient care comes from a host of other providers as well. Skilled nursing facilities (SNFs) and other long-term post-acute care (LTPAC) providers, as well as physical, occupational, behavioral and other therapists, contribute on a regular (and sometimes daily) basis. Additionally, emergency medical services (EMS) also make critical contributions under the most difficult circumstances, which means that the information they accumulate is vital to understanding the patient’s full health picture.
The problem is that these organizations were not included in the financial incentives to transition to an EHR, leading to slower adoption. However, significant progress has been achieved given that 64 percent of SNFs were using an EHR in 2016. Unfortunately, this broader EHR adoption has not completely addressed the need to connect the entire community of care effectively. In fact, despite nearly two-thirds of SNFs having deployed an EHR system, only 30 percent electronically exchange vital clinical data. This remaining reliance on non-electronic transmittal (e.g. fax) of patient data impedes transparency, is time-consuming and introduces the possibility of data entry errors – essentially everything that the HITECH Act was trying to eliminate by requiring EHRs.
Now that we are well on a path toward value-based care and its focus on outcomes and shared risk, it’s more imperative than ever that all providers throughout the continuum have proper transparency around all care being delivered everywhere. It’s the key to reducing unplanned hospital readmissions and emergency department utilization, shortening lengths of stay and ultimately keeping patients (as well as bottom lines) healthier.
 Three Fundamental Requirements for Interoperability
Three Fundamental Requirements for Interoperability
One of the barriers to enabling this last mile of interoperability is the cost factor. Many LTPAC and other post-acute providers operate on extremely thin margins. They simply cannot afford to connect with all the providers in their ecosystem with the type of point-to-point HL7 integration project that hospitals and health systems have done historically.
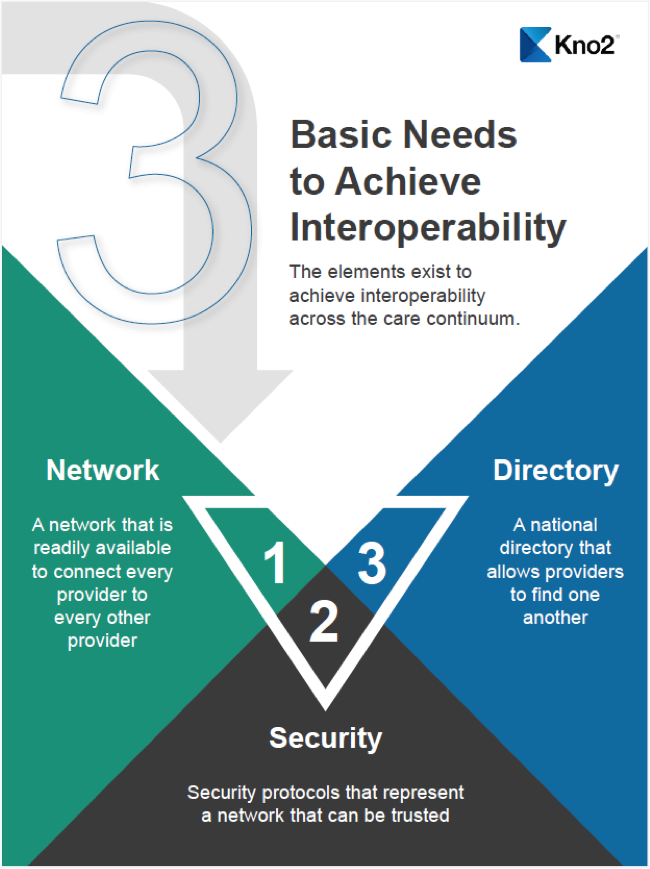
When you break it down, however, there is a much faster and more affordable way to turn on interoperability. At its most basic, interoperability requires three fundamental elements.
- A network that is readily available to connect every provider to every other provider. Think about email. As long as two people both have email applications and an internet connection, the technical hurdle has been removed.
- Security protocols that represent a network that can be trusted. The network must be governed to ensure that data being exchanged is secure, and to provide the assurance that those who are participating on the network are there for the sole purpose of treating patients.
Violating regulations around protected health information and privacy requirements carries specific penalties. No healthcare organization wants to risk that, so if the network cannot be demonstrated to be secure, it won’t be used.
- A national directory that allows providers to find each other, regardless of the forms of communication or technology that they are using to exchange documentation. It’s like a virtual phone book, except that it is available seamlessly within both parties’ normal workflows rather than as a separate source that must be accessed.
All three components must be present to be successful. After all, the most technologically advanced and secure network in the world does little good if a provider can’t find the other members of a patient’s care team and securely exchange critical patient information. Having a directory and governance offers little benefit if there is no mechanism to exchange the information. Additionally, if there is no security, no one will use the system, no matter how easy and convenient it is.
Making Interoperability More Accessible
Once all three fundamental components are in place, broad-based interoperability is achievable. It is then time to start bringing unconnected providers into the network because the patient care chain is only as strong as its weakest link. If any part of the chain is missing, such as patient information from a SNF, the entire chain is broken.
So rather than attempting to impose a separate, costly and complex “interoperability solution” on these highly diversified, resource-constrained providers, the better approach to solving the last mile of interoperability conundrum is to build these capabilities into the technologies and tools they already use.
In some cases, those technologies may be an EHR or practice management system that focuses on the continuum of care. It could also be functionality added to devices that they’re already using, such as a multi-function printer, enabling that device to participate on the same network, using the same security protocols and with the ability to access the same national directory.
The key is that there are organizations that already have trusted relationships with LTPAC, EMS and other providers that were not impacted the HITECH Act. If you can create an interoperability solution that those providers can just “turn on” quickly, easily, securely and at a low cost – all within their normal workflows – then I would say you will have solved much of the challenge of creating a universal, longitudinal health record for every patient.
The Time is Now
Achieving interoperability across all points in the care continuum is essential to improving care quality and health outcomes, lowering costs and supporting a successful transition to value-based care. All the elements exist. Let’s make 2018 the year that we carry it out to the last mile.